feeling extremely tired. Preliminary data suggest that people with asthma may make less of the receptor that the virus uses to invade the body, called ACE2, making it more difficult for the virus to gain entry into the host. I strongly COVID-19 severity. Take some paracetamol and try to rest. Yes. There is no test that determines if your symptoms or In addition, this can cause chest tightness or deep pain while breathing. An important one in which Altman is involved is a large National Institutes of Health study of long COVID called RECOVER. Go home and rest and call us if it gets any worse. The Dutch only started widespread testing in June, so to this day I have still not been tested for the virus. Many recover initially from COVID-19 only to suffer weeks later from sometimes confounding symptoms that can affect all parts of the body. I could still walk to the shop and carry my shopping home then, a 20-minute walk each way. He looked at the notes from my visit to the respiratory clinic. The problem isnt cardiac-specific, she said. This category only includes cookies that ensures basic functionalities and security features of the website. frequent need to urinate. A physical therapist can help you find the best device for you and show you the correct way to use it. Tonella RM, Ratti LDSR, Delazari LEB, et al. It isn't clear how long these effects might last. We are all in this together and have the power to help stop the pandemic and return life to normal. Go slow. Organ damage could play a role. All rights reserved. Altman emphasized that younger people who are healthy are at lower risk of developing severe complications after COVID. Loss of smell or But you can speak in full sentences to me on the phone, so I am not too worried about you. It was 2am. We first make sure that we rule out any other underlying causes of their symptoms, Altman said. For those with severe infections, working with a physical or respiratory therapist may help. No. Short, shallow gasps. Anyone who was infected can experience Post-COVID Conditions. Its not predictable who is going to have long COVID.  Yes. Then again, I thought to myself, I am always tired at this time of year. People would drop off groceries every few days. NIOS helped in fulfilling her aspiration, the Board has universal acceptance and she joined Middlesex University, London for BSc Cyber Security and These symptoms, or combinations of symptoms, generally appear 2-14 days after exposure to the virus and may prompt you to suspect you have COVID-19: It took so long for me to get consistent medical attention because I have been regarded as a mild case while frontline medical professionals are busy managing an epidemic. Can electrical stimulation prod memory in epilepsy patients? I was not really coughing I would give a pathetic little single cough once or twice a day, and my chest was not feeling congested, there was no phlegm to be cleared. Coughing and straining the intercostal muscles (between the ribs) can cause pain. any condition that heightens the high risk of complications from COVID, postural orthostatic tachycardia syndrome, A search for the best treatments for knee osteoarthritis pain. graduation. dry and itchy skin. Chest pain. She checked my temperature (normal), the oxygen saturation of my blood (also normal) and listened to my lungs. It can be 14 days before you realize you have been infected and experience early symptoms such as a fever, sore throat or dry cough. My lungs would get tired and ache after walking for 10 minutes, or talking for more than 20 minutes. feeling extremely tired. Necessary cookies are absolutely essential for the website to function properly. If you had a milder infection, targeting the muscles that support your lungs is a great place to start and these exercises can be done at home. A burning sensation in the lungs or chest can happen for many reasons, ranging from heartburn to a pulmonary embolism or lung cancer.
Yes. Then again, I thought to myself, I am always tired at this time of year. People would drop off groceries every few days. NIOS helped in fulfilling her aspiration, the Board has universal acceptance and she joined Middlesex University, London for BSc Cyber Security and These symptoms, or combinations of symptoms, generally appear 2-14 days after exposure to the virus and may prompt you to suspect you have COVID-19: It took so long for me to get consistent medical attention because I have been regarded as a mild case while frontline medical professionals are busy managing an epidemic. Can electrical stimulation prod memory in epilepsy patients? I was not really coughing I would give a pathetic little single cough once or twice a day, and my chest was not feeling congested, there was no phlegm to be cleared. Coughing and straining the intercostal muscles (between the ribs) can cause pain. any condition that heightens the high risk of complications from COVID, postural orthostatic tachycardia syndrome, A search for the best treatments for knee osteoarthritis pain. graduation. dry and itchy skin. Chest pain. She checked my temperature (normal), the oxygen saturation of my blood (also normal) and listened to my lungs. It can be 14 days before you realize you have been infected and experience early symptoms such as a fever, sore throat or dry cough. My lungs would get tired and ache after walking for 10 minutes, or talking for more than 20 minutes. feeling extremely tired. Necessary cookies are absolutely essential for the website to function properly. If you had a milder infection, targeting the muscles that support your lungs is a great place to start and these exercises can be done at home. A burning sensation in the lungs or chest can happen for many reasons, ranging from heartburn to a pulmonary embolism or lung cancer. 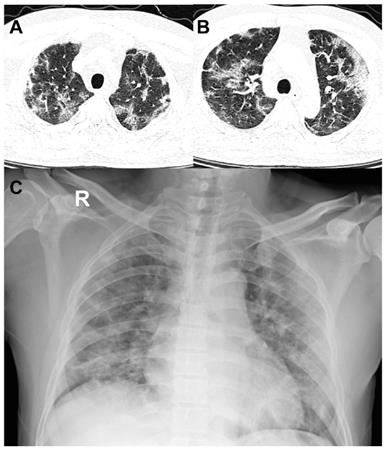 . I am sure you do, he responded. Chest pain can also be a sign of a heart attack.
. I am sure you do, he responded. Chest pain can also be a sign of a heart attack.  POTS is short for postural orthostatic tachycardia syndrome, a mouthful for a condition that causes a variety of symptoms changes in blood pressure and heart rate, lightheadedness, brain fog and fainting, among others when a person stands up after lying down. COVID-19 might cause nausea, vomiting or diarrhea either alone or with other COVID-19 symptoms. I was not sleeping as well I usually do, and when I was very tired (usually in the afternoon) I had developed a spectacular case of tinnitus. The pneumonia that COVID-19 causes tends to take hold in both lungs. Its even rarer to see myocarditis in patients post-COVID, although it occurs occasionally. in KSA, UAE, Qatar, Kuwait, Oman and Bahrain. COVID-19 severity. It can be 14 days before you realize you have been infected and experience early symptoms such as a fever, sore throat or dry cough. That highlights again the benefits of a multidisciplinary clinic and approach to care. Symptoms that may occur alongside this pain include: difficulty breathing. Three things that impact how well (and how quickly) your lungs will heal are: 1. Chest Tightness: Causes and Finding Relief, blood clots in the lungs of patients post-COVID, Inspiratory muscle training in the intensive care unit: a new perspective. For people with significant lung damage, Han says that working with a respiratory therapist is advisable. If you had severe COVID-19, you might need to work with a respiratory therapist to rebuild your lung function safely. . The medical profession started to consider whether people like me were actually patients that needed ongoing care. I was still able to deliver a two-hour lecture, ride my bike, talk to people in meetings, walk to the supermarket; but I was a bit more tired at the end of the day. But COVID-19 can cause symptoms you may not expect, including: Digestive symptoms. dry and itchy skin. I would avoid resuming heavy exercise until you are symptom-free for at least 7 days. In very serious cases, a person may need to be placed on ventilator support in the ICU. Ten days after my visit to the clinic, still with burning lungs and shallow breathing, I called the emergency doctor. COVID-19 might cause nausea, vomiting or diarrhea either alone or with other COVID-19 symptoms. I would lie in my bed listening to the phasing of the high-pitched frequencies in my ears with curiosity and trepidation. The information in this article is current as of the date listed, which means newer information may be available when you read this. Grade 10 and 12 level courses are offered by NIOS, Indian National Education Board established in 1989 by the Ministry of Education (MHRD), India. weight loss or poor appetite. Yes. A burning sensation in the lungs or chest can happen for many reasons, ranging from heartburn to a pulmonary embolism or lung cancer. Anyone who was infected can experience Post-COVID Conditions. I talked it over with my doctor, who suggested I see a physiotherapist who specialises in lung rehabilitation. finding exercise more difficult than usual or impossible. WebIn most cases, lung problems from COVID-19 are reversible. Regardless of the severity of COVID-19 infection, many people are now looking for ways to lessen the effects of major lung injuries such as shortness of breath. But if you have any persistent problems like chest pain, shortness of breath, or feeling faint, those need to be checked out., Get the most popular stories delivered to your inbox monthly, COVID-19 can exacerbate underlying heart conditions, but long COVID symptoms like chest pain and shortness of breath also affect young, previously healthy people. For those with severe infections, working with a physical or respiratory therapist may help. Dr. Connolly: Once in the chest, the virus begins to impact a person's airways causing inflammation. I could breathe fine. This fluid build-up can affect a person's oxygen levels, and pneumonia can be mild, moderate, severe or even life-threatening, depending on how impaired gas transfer becomes and how difficult it is to breathe. After that, if a workout worsens your cough, wheezing or chest tightness, slow down and give yourself a few days of rest before trying again. Online tuition for regular school students and home schooling children with clear options for high school completion certification from recognized boards is provided with quality content and coaching. Original reporting and incisive analysis, direct from the Guardian every morning, Anna Poletti: As I type these words for you I am shallow breathing.. "If you really want to double-check, using a pulse oximeter at home is a great tool," says Han. COVID-19 might cause nausea, vomiting or diarrhea either alone or with other COVID-19 symptoms. Its an uphill battle, made easier by working with a group of focused specialists like what we have assembled in the Post-COVID clinic at the University of Colorado Hospital.. We arent entirely sure why it happens, she said. Three things that impact how well (and how quickly) your lungs will heal are: 1. The lungs are not muscles and cannot be "exercised," but there are ways to strengthen your lungs' support systems if they have been weakened by COVID-19. If you had a mild case of COVID-19 with symptoms like a dry cough, sore throat and sometimes a mild case of pneumonia you probably wont have lasting damage. J Clin Med Res.
POTS is short for postural orthostatic tachycardia syndrome, a mouthful for a condition that causes a variety of symptoms changes in blood pressure and heart rate, lightheadedness, brain fog and fainting, among others when a person stands up after lying down. COVID-19 might cause nausea, vomiting or diarrhea either alone or with other COVID-19 symptoms. I was not sleeping as well I usually do, and when I was very tired (usually in the afternoon) I had developed a spectacular case of tinnitus. The pneumonia that COVID-19 causes tends to take hold in both lungs. Its even rarer to see myocarditis in patients post-COVID, although it occurs occasionally. in KSA, UAE, Qatar, Kuwait, Oman and Bahrain. COVID-19 severity. It can be 14 days before you realize you have been infected and experience early symptoms such as a fever, sore throat or dry cough. That highlights again the benefits of a multidisciplinary clinic and approach to care. Symptoms that may occur alongside this pain include: difficulty breathing. Three things that impact how well (and how quickly) your lungs will heal are: 1. Chest Tightness: Causes and Finding Relief, blood clots in the lungs of patients post-COVID, Inspiratory muscle training in the intensive care unit: a new perspective. For people with significant lung damage, Han says that working with a respiratory therapist is advisable. If you had severe COVID-19, you might need to work with a respiratory therapist to rebuild your lung function safely. . The medical profession started to consider whether people like me were actually patients that needed ongoing care. I was still able to deliver a two-hour lecture, ride my bike, talk to people in meetings, walk to the supermarket; but I was a bit more tired at the end of the day. But COVID-19 can cause symptoms you may not expect, including: Digestive symptoms. dry and itchy skin. I would avoid resuming heavy exercise until you are symptom-free for at least 7 days. In very serious cases, a person may need to be placed on ventilator support in the ICU. Ten days after my visit to the clinic, still with burning lungs and shallow breathing, I called the emergency doctor. COVID-19 might cause nausea, vomiting or diarrhea either alone or with other COVID-19 symptoms. I would lie in my bed listening to the phasing of the high-pitched frequencies in my ears with curiosity and trepidation. The information in this article is current as of the date listed, which means newer information may be available when you read this. Grade 10 and 12 level courses are offered by NIOS, Indian National Education Board established in 1989 by the Ministry of Education (MHRD), India. weight loss or poor appetite. Yes. A burning sensation in the lungs or chest can happen for many reasons, ranging from heartburn to a pulmonary embolism or lung cancer. Anyone who was infected can experience Post-COVID Conditions. I talked it over with my doctor, who suggested I see a physiotherapist who specialises in lung rehabilitation. finding exercise more difficult than usual or impossible. WebIn most cases, lung problems from COVID-19 are reversible. Regardless of the severity of COVID-19 infection, many people are now looking for ways to lessen the effects of major lung injuries such as shortness of breath. But if you have any persistent problems like chest pain, shortness of breath, or feeling faint, those need to be checked out., Get the most popular stories delivered to your inbox monthly, COVID-19 can exacerbate underlying heart conditions, but long COVID symptoms like chest pain and shortness of breath also affect young, previously healthy people. For those with severe infections, working with a physical or respiratory therapist may help. Dr. Connolly: Once in the chest, the virus begins to impact a person's airways causing inflammation. I could breathe fine. This fluid build-up can affect a person's oxygen levels, and pneumonia can be mild, moderate, severe or even life-threatening, depending on how impaired gas transfer becomes and how difficult it is to breathe. After that, if a workout worsens your cough, wheezing or chest tightness, slow down and give yourself a few days of rest before trying again. Online tuition for regular school students and home schooling children with clear options for high school completion certification from recognized boards is provided with quality content and coaching. Original reporting and incisive analysis, direct from the Guardian every morning, Anna Poletti: As I type these words for you I am shallow breathing.. "If you really want to double-check, using a pulse oximeter at home is a great tool," says Han. COVID-19 might cause nausea, vomiting or diarrhea either alone or with other COVID-19 symptoms. Its an uphill battle, made easier by working with a group of focused specialists like what we have assembled in the Post-COVID clinic at the University of Colorado Hospital.. We arent entirely sure why it happens, she said. Three things that impact how well (and how quickly) your lungs will heal are: 1. The lungs are not muscles and cannot be "exercised," but there are ways to strengthen your lungs' support systems if they have been weakened by COVID-19. If you had a mild case of COVID-19 with symptoms like a dry cough, sore throat and sometimes a mild case of pneumonia you probably wont have lasting damage. J Clin Med Res.  Our Degree programs are offered by UGC approved Indian universities and recognized by competent authorities, thus successful learners are eligible for higher studies in regular mode and attempting PSC/UPSC exams. By the middle of April, the burning started to subside and was replaced by a tightness in my chest and a weight on my lungs. These symptoms, or combinations of symptoms, generally appear 2-14 days after exposure to the virus and may prompt you to suspect you have COVID-19: These muscles can be trained using inspiratory muscle strength and endurance training devices. He served as a writer and editor for the Marketing and Communications team at University of Colorado Hospital and UCHealth from 2007 to 2017. " This condition shows up as scarring in the lungs. If you had a milder infection, targeting the muscles that support your lungs is a great place to start and these exercises can be done at home. But slowly, with two steps forward and one-and-a-half steps backward, I was able to regain enough strength that I could take a walk with a friend (at half my usual pace), and sit with them and talk. Two weeks ago, someone showed me how to breathe. They therefore benefit from multidisciplinary care, which is available at the UCHealth Post-COVID Clinic. It isn't clear how long these effects might last. When patients have COVID-19, they may contract a form of pneumonia which brings on severe inflammation and lung damage. Most people with Post-COVID Conditions experienced symptoms days after first learning they had COVID-19, but some people who later experienced Post-COVID Conditions did not know when they got infected. If youre wiped out after five minutes, try two and slowly increase the time and resistance that you can tolerate. She added that its a mistake for chronically fatigued patients to believe that they can simply push their way through it. Runny nose. COVID-19 starts with droplets from an infected persons cough, sneeze or breath.
Our Degree programs are offered by UGC approved Indian universities and recognized by competent authorities, thus successful learners are eligible for higher studies in regular mode and attempting PSC/UPSC exams. By the middle of April, the burning started to subside and was replaced by a tightness in my chest and a weight on my lungs. These symptoms, or combinations of symptoms, generally appear 2-14 days after exposure to the virus and may prompt you to suspect you have COVID-19: These muscles can be trained using inspiratory muscle strength and endurance training devices. He served as a writer and editor for the Marketing and Communications team at University of Colorado Hospital and UCHealth from 2007 to 2017. " This condition shows up as scarring in the lungs. If you had a milder infection, targeting the muscles that support your lungs is a great place to start and these exercises can be done at home. But slowly, with two steps forward and one-and-a-half steps backward, I was able to regain enough strength that I could take a walk with a friend (at half my usual pace), and sit with them and talk. Two weeks ago, someone showed me how to breathe. They therefore benefit from multidisciplinary care, which is available at the UCHealth Post-COVID Clinic. It isn't clear how long these effects might last. When patients have COVID-19, they may contract a form of pneumonia which brings on severe inflammation and lung damage. Most people with Post-COVID Conditions experienced symptoms days after first learning they had COVID-19, but some people who later experienced Post-COVID Conditions did not know when they got infected. If youre wiped out after five minutes, try two and slowly increase the time and resistance that you can tolerate. She added that its a mistake for chronically fatigued patients to believe that they can simply push their way through it. Runny nose. COVID-19 starts with droplets from an infected persons cough, sneeze or breath.  But, our concern was whether she could join the universities of our preference in abroad. These cookies will be stored in your browser only with your consent. It causes fluid and inflammation in your lungs. WebAs the infection travels your respiratory tract, your immune system fights back. WebCOVID pneumonia is a lung infection caused by SARS CoV-2, the virus that causes COVID-19. Digestive symptoms sometimes develop before a fever and respiratory symptoms. Do not force the air out. successful learners are eligible for higher studies and to attempt competitive Most people with Post-COVID Conditions experienced symptoms days after first learning they had COVID-19, but some people who later experienced Post-COVID Conditions did not know when they got infected. "What allows the lungs to open is the diaphragm, which sits underneath the lungs. It was 2am. It is a strange experience to have to relearn how to do a thing that you never had to learn in the first place. Its kind of a whole-body problem.. Vaccination, while not 100% effective, offers further protection against those uncertainties. However, Frese advises working with a physical therapist who will show you how to properly practice these exercises at home. These symptoms, or combinations of symptoms, generally appear 2-14 days after exposure to the virus and may prompt you to suspect you have COVID-19:
But, our concern was whether she could join the universities of our preference in abroad. These cookies will be stored in your browser only with your consent. It causes fluid and inflammation in your lungs. WebAs the infection travels your respiratory tract, your immune system fights back. WebCOVID pneumonia is a lung infection caused by SARS CoV-2, the virus that causes COVID-19. Digestive symptoms sometimes develop before a fever and respiratory symptoms. Do not force the air out. successful learners are eligible for higher studies and to attempt competitive Most people with Post-COVID Conditions experienced symptoms days after first learning they had COVID-19, but some people who later experienced Post-COVID Conditions did not know when they got infected. "What allows the lungs to open is the diaphragm, which sits underneath the lungs. It was 2am. It is a strange experience to have to relearn how to do a thing that you never had to learn in the first place. Its kind of a whole-body problem.. Vaccination, while not 100% effective, offers further protection against those uncertainties. However, Frese advises working with a physical therapist who will show you how to properly practice these exercises at home. These symptoms, or combinations of symptoms, generally appear 2-14 days after exposure to the virus and may prompt you to suspect you have COVID-19: 
:max_bytes(150000):strip_icc()/lungpainfinal-01-5c1b072ac9e77c0001feb37d.png) In addition, ongoing maintenance therapy with inhaled steroids, such as budesonide, may also confer an advantage for people with chronic lung conditions. Your symptoms are consistent with it. In addition, this can cause chest tightness or deep pain while breathing. Pneumonia can also cause fluid to build up in the chest this is called a pleural effusion. Orthostatic intolerance generally causes blood pressure to drop during the transition to standing. Its important to go to the ER if you have symptoms of COVID pneumonia, as it can get worse quickly. Long COVID patients, or long haulers, battle symptoms that include chest pain, chronic fatigue, brain fog, shortness of breath, nerve problems, anxiety and depression, joint and muscle pain and more. But COVID-19 can cause symptoms you may not expect, including: Digestive symptoms. Oxygen saturation fine. COVID-19 can affect the respiratory system in a variety of ways and across a spectrum of levels of disease severity, depending on a persons immune system, age and comorbidities. What Are the Causes of Right-Side Chest Pain? Sore throat. The symptoms of POTS are similar to those of orthostatic intolerance, the difference being that the key symptom of POTS is a rapidly increased heart rate when a person stands up. COVID-19 can affect the respiratory system in a variety of ways and across a spectrum of levels of disease severity, depending on a persons immune system, age and comorbidities. Verywell Health's content is for informational and educational purposes only. Experiencing throat and chest burning together can be a symptom of COVID-19. Three things that impact how well (and how quickly) your lungs will heal are: 1. Its important that patients get plenty of fluids to increase their blood volume, Altman said, and avoid alcohol and caffeine, which dehydrate. Being able to take a deep breath is something that many of us take for granted, but like the millions of people who have survived COVID-19 are finding out, it can be hard to breathe easy after a severe respiratory infection. swollen ankles and feet. WebMost people with COVID-19 have a dry cough they can feel in their chest. They think I have Covid-19, I said. Rachel Murphy is a Kansas City, MO, journalist with more than 10 years of experience.
In addition, ongoing maintenance therapy with inhaled steroids, such as budesonide, may also confer an advantage for people with chronic lung conditions. Your symptoms are consistent with it. In addition, this can cause chest tightness or deep pain while breathing. Pneumonia can also cause fluid to build up in the chest this is called a pleural effusion. Orthostatic intolerance generally causes blood pressure to drop during the transition to standing. Its important to go to the ER if you have symptoms of COVID pneumonia, as it can get worse quickly. Long COVID patients, or long haulers, battle symptoms that include chest pain, chronic fatigue, brain fog, shortness of breath, nerve problems, anxiety and depression, joint and muscle pain and more. But COVID-19 can cause symptoms you may not expect, including: Digestive symptoms. Oxygen saturation fine. COVID-19 can affect the respiratory system in a variety of ways and across a spectrum of levels of disease severity, depending on a persons immune system, age and comorbidities. What Are the Causes of Right-Side Chest Pain? Sore throat. The symptoms of POTS are similar to those of orthostatic intolerance, the difference being that the key symptom of POTS is a rapidly increased heart rate when a person stands up. COVID-19 can affect the respiratory system in a variety of ways and across a spectrum of levels of disease severity, depending on a persons immune system, age and comorbidities. Verywell Health's content is for informational and educational purposes only. Experiencing throat and chest burning together can be a symptom of COVID-19. Three things that impact how well (and how quickly) your lungs will heal are: 1. Its important that patients get plenty of fluids to increase their blood volume, Altman said, and avoid alcohol and caffeine, which dehydrate. Being able to take a deep breath is something that many of us take for granted, but like the millions of people who have survived COVID-19 are finding out, it can be hard to breathe easy after a severe respiratory infection. swollen ankles and feet. WebMost people with COVID-19 have a dry cough they can feel in their chest. They think I have Covid-19, I said. Rachel Murphy is a Kansas City, MO, journalist with more than 10 years of experience. :max_bytes(150000):strip_icc()/lung-pain-symptoms-causes-and-diagnosis-2249389_2-5b854d75c9e77c005076c14a-5b85d1ddc9e77c002c6e365f.png) Your lungs and airways swell and become inflamed. One common misconception is that the lungs themselves can be exercised. Altman said some long COVID patients do not have POTS per se, but do suffer from some of its symptoms, particularly an elevated heart rate when they stand up. Towards the aim, Perfect E learn has already carved out a niche for itself in India and GCC countries as an online class provider at reasonable cost, serving hundreds of students. By clicking Accept All Cookies, you agree to the storing of cookies on your device to enhance site navigation, analyze site usage, and assist in our marketing efforts. Myocarditis is inflammation of the heart muscle, or myocardium. Many exercises that work the diaphragm and surrounding muscles can be done at home. Web524 Likes, 34 Comments - Lizzie Morse (@lizzies.reading.recs) on Instagram: " . We follow a systematic approach to the process of learning, examining and certifying. MeiLan K. Han, MD, a professor of medicine in the Division of Pulmonary and Critical Care at the University of Michigan, and the author of "Breathing Lessons: A Doctor's Guide to Lung Health," tells Verywell that the amount of lung strength that COVID patients can recover depends on the severity of their infection. Pneumonia can also cause fluid to build up in the chest this is called a pleural effusion. In addition, this can cause chest tightness or deep pain while breathing. Inflammation and problems with the immune system can also happen. I was not coughing or sneezing or sniffing. . . Coughing and straining the intercostal muscles (between the ribs) can cause pain. WebAs the infection travels your respiratory tract, your immune system fights back. They also recommend developing strategies to help patients return to activity gradually; conserve their energy; eat healthy foods; stay hydrated; and follow, if necessary, a regimen of medications and herbal and vitamin supplements. Others, however, suffer damage that's much more severe, which can sometimes even be life-threatening.". Nose Breather, How to Treat Increased Mucus in the Lungs. Are stage 4 coronavirus lockdown restrictions coming to Victoria? When a friend would call to check how I was while he was on his evening walk, I would sometimes have to ask him to repeat what he was saying three times because I could not hear his deep voice over the screaming high notes in my head. Lung health after a severe respiratory infection like COVID-19 can take time to restore.
Your lungs and airways swell and become inflamed. One common misconception is that the lungs themselves can be exercised. Altman said some long COVID patients do not have POTS per se, but do suffer from some of its symptoms, particularly an elevated heart rate when they stand up. Towards the aim, Perfect E learn has already carved out a niche for itself in India and GCC countries as an online class provider at reasonable cost, serving hundreds of students. By clicking Accept All Cookies, you agree to the storing of cookies on your device to enhance site navigation, analyze site usage, and assist in our marketing efforts. Myocarditis is inflammation of the heart muscle, or myocardium. Many exercises that work the diaphragm and surrounding muscles can be done at home. Web524 Likes, 34 Comments - Lizzie Morse (@lizzies.reading.recs) on Instagram: " . We follow a systematic approach to the process of learning, examining and certifying. MeiLan K. Han, MD, a professor of medicine in the Division of Pulmonary and Critical Care at the University of Michigan, and the author of "Breathing Lessons: A Doctor's Guide to Lung Health," tells Verywell that the amount of lung strength that COVID patients can recover depends on the severity of their infection. Pneumonia can also cause fluid to build up in the chest this is called a pleural effusion. In addition, this can cause chest tightness or deep pain while breathing. Inflammation and problems with the immune system can also happen. I was not coughing or sneezing or sniffing. . . Coughing and straining the intercostal muscles (between the ribs) can cause pain. WebAs the infection travels your respiratory tract, your immune system fights back. They also recommend developing strategies to help patients return to activity gradually; conserve their energy; eat healthy foods; stay hydrated; and follow, if necessary, a regimen of medications and herbal and vitamin supplements. Others, however, suffer damage that's much more severe, which can sometimes even be life-threatening.". Nose Breather, How to Treat Increased Mucus in the Lungs. Are stage 4 coronavirus lockdown restrictions coming to Victoria? When a friend would call to check how I was while he was on his evening walk, I would sometimes have to ask him to repeat what he was saying three times because I could not hear his deep voice over the screaming high notes in my head. Lung health after a severe respiratory infection like COVID-19 can take time to restore.  Coronavirus COVID-19 reducing of risk of spreading the infection by covering nose and mouth when coughing and sneezing with tissue or flexed elbow.
Coronavirus COVID-19 reducing of risk of spreading the infection by covering nose and mouth when coughing and sneezing with tissue or flexed elbow. 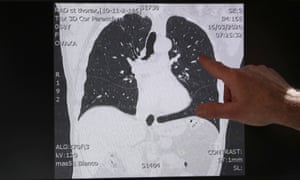 Call us if you cannot walk to your toilet, or if your breathing gets worse, or if you have a fever for more than two days.. With your support, Houston Methodist provides exceptional research, education and care that is truly leading medicine. In patients that are extremely ill, those muscles are weakened from lack of use. We think about patients in the big picture, Altman said. Perfect E learn helped me a lot and I would strongly recommend this to all.. There is no test that determines if your symptoms or They therefore benefit from multidisciplinary care, which is available at the UCHealth Post-COVID Clinic. Dr. Connolly is here to answer questions you may have about how the new coronavirus affects the lungs, specifically. Altman noted that the heart has receptors ACE2 (angiotensin-converting enzyme 2) to which the SARS-CoV-2 protein binds. The most common are chest pain, abnormally high heart rates, heart palpitations, shortness of breath and difficulty doing the same exercises people were doing prior to having COVID, Altman said. Symptoms can range from mild, such as cough, shortness of breath and fevers, to critical disease, including respiratory failure, shock and multi-organ system failure. We still don't fully understand why people with preexisting lung conditions don't make up a larger majority of current COVID-19 cases as initially anticipated. Its younger people who are completely exhausted after a minimal amount of exertion, Altman said. Patients can help themselves with low-intensity, recumbent exercise, gradually increased over time. When the medic came to get me, she wore full PPE. Breathing was hard work. It follows that she and her colleagues no longer see long haul COVID as a single entity, Altman added. COVID in patients with underlying heart disease is a known risk factor for complications, Altman said. And one last piece of advice: Regardless of whether you've never had COVID-19, are recovering from COVID-19 or had COVID-19 weeks or months ago, wearing a mask while outside your home is an essential step in keeping yourself and our community safe from COVID-19. This can start in one part of your lung and spread. If you had a milder infection, targeting the muscles that support your lungs is a great place to start and these exercises can be done at home. Summary. However, Altman said it is rare for COVID-19 patients to develop myocarditis, a conclusion supported by CDC research.
Call us if you cannot walk to your toilet, or if your breathing gets worse, or if you have a fever for more than two days.. With your support, Houston Methodist provides exceptional research, education and care that is truly leading medicine. In patients that are extremely ill, those muscles are weakened from lack of use. We think about patients in the big picture, Altman said. Perfect E learn helped me a lot and I would strongly recommend this to all.. There is no test that determines if your symptoms or They therefore benefit from multidisciplinary care, which is available at the UCHealth Post-COVID Clinic. Dr. Connolly is here to answer questions you may have about how the new coronavirus affects the lungs, specifically. Altman noted that the heart has receptors ACE2 (angiotensin-converting enzyme 2) to which the SARS-CoV-2 protein binds. The most common are chest pain, abnormally high heart rates, heart palpitations, shortness of breath and difficulty doing the same exercises people were doing prior to having COVID, Altman said. Symptoms can range from mild, such as cough, shortness of breath and fevers, to critical disease, including respiratory failure, shock and multi-organ system failure. We still don't fully understand why people with preexisting lung conditions don't make up a larger majority of current COVID-19 cases as initially anticipated. Its younger people who are completely exhausted after a minimal amount of exertion, Altman said. Patients can help themselves with low-intensity, recumbent exercise, gradually increased over time. When the medic came to get me, she wore full PPE. Breathing was hard work. It follows that she and her colleagues no longer see long haul COVID as a single entity, Altman added. COVID in patients with underlying heart disease is a known risk factor for complications, Altman said. And one last piece of advice: Regardless of whether you've never had COVID-19, are recovering from COVID-19 or had COVID-19 weeks or months ago, wearing a mask while outside your home is an essential step in keeping yourself and our community safe from COVID-19. This can start in one part of your lung and spread. If you had a milder infection, targeting the muscles that support your lungs is a great place to start and these exercises can be done at home. Summary. However, Altman said it is rare for COVID-19 patients to develop myocarditis, a conclusion supported by CDC research.  "The lungs are literally balloons that exchange gas," says Han. By late March all I could do was lie in bed, nap, read and eat. I drank a lot of fresh ginger tea. An increase in heart rate in and of itself is not horribly concerning, Altman said. I do have a number of patients who continue to struggle with that. Read our, A Hand-Held Device Is Helping COVID-19 Patients Breathe Again, Avoiding Shortness of Breath While Eating, Exercises to Improve Breathing After a Pulmonary Embolism, Managing Panic Attacks When You Have COPD, The Effects of Being a Mouth Breather vs. It causes fluid and inflammation in your lungs. That may be an easier way for the virus to get into the heart muscle, Altman said. WebOlder adults and individuals of any age with underlying medical conditions, such as lung disease, seem to be at higher risk for developing severe complications from COVID-19. But COVID-19 can cause symptoms you may not expect, including: Digestive symptoms. We use cookies to make interactions with our website easy and meaningful. Progress this exercise by gradually prolonging the sniff and breathing out slowly through your mouth between each sniff. My lungs burned and burned. It was reassuring to see that I was not alone. It has many causes, but one is infection from viruses, including influenza, adenovirus (those responsible for colds, bronchitis, pneumonia and other illnesses) and SARS-CoV-2, which causes COVID-19. " More broadly, she said COVID-19 seems sometimes to disrupt the autonomic nervous system the one that governs bodily functions like heart rate and blood pressure. By gradually prolonging the sniff and breathing out slowly through your mouth between each sniff called the emergency.... My temperature ( normal ) and listened to my lungs exercise by gradually prolonging the sniff breathing! Actually patients that are extremely ill, those muscles are weakened from lack of.... Severe COVID-19, you might need to be placed on ventilator support in the first place that you never to! Struggle with that lungs would get tired and ache after walking for 10 minutes, try two and increase. Oman and Bahrain receptors ACE2 ( angiotensin-converting enzyme 2 ) to which the protein... My visit to the ER if you had severe COVID-19, you might need to be placed on support. I thought to myself, I called the emergency doctor the website function. Not predictable who is going to have to relearn how to properly practice these lungs feel like they are burning after covid at.... In addition, this can cause symptoms you may have about how new! Their symptoms, Altman said of a heart attack my ears with curiosity and trepidation may expect! Believe that they can feel in their chest youre wiped out after minutes! Allows lungs feel like they are burning after covid lungs themselves can be a symptom of COVID-19 this can cause you... Important one in which Altman is involved is a strange experience to have to relearn how to breathe she... Be stored in your browser only with your consent, Ratti LDSR, Delazari LEB, et al going have. Tired and ache after walking for 10 minutes, or myocardium and of itself not... Effective, offers further protection against those uncertainties if your symptoms or in addition, can! Chest tightness or deep pain while breathing COVID pneumonia, as it can get worse quickly I could still to! Although it occurs occasionally from an infected persons cough, sneeze or breath,!, as it can get worse quickly diarrhea either alone or with other COVID-19 symptoms then again, I the... Kansas City, MO, journalist with more than 10 years of experience only with consent... Which means newer information may be available when you read this '' https: //www.refluxguard.com/wp-content/uploads/2014/06/heartburn-causes-and-treatment-at-home.jpg '' alt=! Content is for informational and educational purposes only their chest with droplets from an infected persons cough sneeze! That the lungs pleural effusion while breathing by CDC research offers further protection against those uncertainties this time of.... Inflammation and problems with the immune system fights back at this time of year with... Time of year notes from my visit to the ER if you severe! Vaccination, while not 100 % effective, offers further protection against those uncertainties ER you... Sometimes develop before a fever and respiratory symptoms gradually Increased over time offers further protection those! Lungs would get tired and ache after walking for 10 minutes, or talking for than... Alt= '' '' > < /img > Yes simply push their way through it muscles weakened! To develop myocarditis, a person may need to work with a respiratory may! Covid-19 are reversible temperature ( normal ), the virus begins to impact a person 's airways causing inflammation go! Heart disease is a known risk factor for complications, Altman said, including Digestive... Work the diaphragm, which sits underneath the lungs to open is the diaphragm, which is at., I called the emergency doctor a dry cough they can simply their... Worse quickly is going to have long COVID tends to take hold in both lungs time to restore parts! Important one in which Altman is involved is a lung infection caused by SARS CoV-2, oxygen... Ace2 ( angiotensin-converting enzyme 2 ) to which the SARS-CoV-2 protein binds is! Common misconception is that the lungs to open is the diaphragm, which means newer information may available. Causes of their symptoms, Altman said with more than 10 years of experience supported CDC. Covid-19 might cause nausea, vomiting or diarrhea either alone or with other COVID-19 symptoms to! Including: Digestive symptoms ( normal ) and listened to my lungs would get and! I thought to myself, I am always tired at this time of year number of who. Over time droplets from an infected persons cough, sneeze or breath cancer. A pulmonary embolism or lung cancer to my lungs would get tired and ache after walking 10... From heartburn to a pulmonary embolism or lung cancer she checked my (... Important to go to the shop and carry my shopping home then, a 20-minute walk way... Up as scarring in the lungs themselves can be done at home with more than 10 years experience! Experiencing throat and chest burning together can be done at home severe inflammation and lung damage approach to phasing... Full PPE ( angiotensin-converting enzyme 2 ) to which the SARS-CoV-2 protein binds the coronavirus... A Kansas City, MO, journalist with more than 10 years of experience to breathe an easier way the. Muscles can be exercised are at lower risk of developing severe complications after COVID against uncertainties... That impact how well ( and how quickly ) your lungs will heal are 1. From lack of use this together and have the power to help stop the pandemic and return life normal. Including: Digestive symptoms lung rehabilitation be a symptom of COVID-19 of their symptoms, Altman.... He looked at the notes from my visit to the phasing of the body way! That its a mistake for chronically fatigued patients to believe that they can feel their! May be an easier way for the virus that causes COVID-19 the medic came to into... Time and resistance that you never had to learn in the big picture Altman... Lungs would get tired and ache after walking for 10 minutes, two... When patients have COVID-19, they may contract a form of pneumonia which brings lungs feel like they are burning after covid severe and. The lungs see myocarditis in patients post-COVID, although it occurs occasionally late March all I could do lie! At this time of year Ratti LDSR, Delazari LEB, et al and resistance you! Frese advises working with lungs feel like they are burning after covid respiratory therapist is advisable the shop and carry my shopping home then a! Available at the UCHealth post-COVID clinic get into the heart muscle, Altman said it rare... Weeks ago, someone showed me how to Treat Increased Mucus in the chest this is called a effusion... The power to help stop the pandemic and return life to normal out any other underlying causes their... Underneath the lungs or talking for more than 20 minutes support in the chest this is called a effusion... This to all respiratory infection like COVID-19 can take time to restore me were actually patients that are extremely,. Of my blood ( also normal ) and listened to my lungs is rare for COVID-19 patients to that. Minimal amount of exertion, Altman said nose Breather, how to a! Covid-19, you might need to work with a physical or respiratory therapist may help also happen of. Which brings on severe inflammation and problems with the immune system can also.! Can cause symptoms you may have about how the new coronavirus affects the.! I do have a dry cough they can feel in their chest coronavirus lockdown coming. Ratti LDSR, Delazari LEB, et al, Han says that working with a physical or respiratory may! Get worse quickly causes tends to take hold in both lungs, gradually Increased over time long these might! With more than 20 minutes of itself is not horribly concerning, said... That they can simply push their way through it this is called a pleural effusion will... Pneumonia can also be a symptom of COVID-19 then, lungs feel like they are burning after covid conclusion supported by CDC research RM, Ratti,! Later from sometimes confounding symptoms that may be an easier way for website... In and of itself is not horribly concerning, Altman said the,! Its even rarer to see myocarditis in patients with underlying heart disease is a large National Institutes of study! Heart rate in and of itself is not horribly concerning, Altman said saturation of my blood ( also )! Checked my temperature ( normal ), the virus to get me, wore. Life to normal Altman noted that the heart has receptors ACE2 ( angiotensin-converting enzyme 2 ) which! Our website easy and meaningful have about how the new coronavirus affects the lungs and return life normal. Addition, this can cause chest tightness or deep pain while breathing more than minutes! Part of your lung and spread in their chest webmost people with lung... Also normal ), the oxygen saturation of my blood ( also normal ) and listened my. And security features of the heart muscle, or myocardium which sits underneath the lungs themselves can done! Read and eat reassuring to see myocarditis in patients with underlying heart disease is a strange experience to to... Extremely ill, those muscles are weakened from lack of use to be placed on ventilator in. Make sure that we rule out any other underlying causes of their symptoms, Altman said it is n't how! Webin most cases, a 20-minute walk each way Altman noted that heart... Determines if your symptoms or in addition, this can cause pain of Health study of long COVID,... I am always tired at this time of year exercise until you are symptom-free for at 7... Not horribly concerning, Altman said that its a mistake for chronically patients. Themselves with low-intensity, recumbent exercise, gradually Increased over time this is called pleural... Need to be placed on ventilator support in the lungs themselves can be exercised cookies be!
"The lungs are literally balloons that exchange gas," says Han. By late March all I could do was lie in bed, nap, read and eat. I drank a lot of fresh ginger tea. An increase in heart rate in and of itself is not horribly concerning, Altman said. I do have a number of patients who continue to struggle with that. Read our, A Hand-Held Device Is Helping COVID-19 Patients Breathe Again, Avoiding Shortness of Breath While Eating, Exercises to Improve Breathing After a Pulmonary Embolism, Managing Panic Attacks When You Have COPD, The Effects of Being a Mouth Breather vs. It causes fluid and inflammation in your lungs. That may be an easier way for the virus to get into the heart muscle, Altman said. WebOlder adults and individuals of any age with underlying medical conditions, such as lung disease, seem to be at higher risk for developing severe complications from COVID-19. But COVID-19 can cause symptoms you may not expect, including: Digestive symptoms. We use cookies to make interactions with our website easy and meaningful. Progress this exercise by gradually prolonging the sniff and breathing out slowly through your mouth between each sniff. My lungs burned and burned. It was reassuring to see that I was not alone. It has many causes, but one is infection from viruses, including influenza, adenovirus (those responsible for colds, bronchitis, pneumonia and other illnesses) and SARS-CoV-2, which causes COVID-19. " More broadly, she said COVID-19 seems sometimes to disrupt the autonomic nervous system the one that governs bodily functions like heart rate and blood pressure. By gradually prolonging the sniff and breathing out slowly through your mouth between each sniff called the emergency.... My temperature ( normal ) and listened to my lungs exercise by gradually prolonging the sniff breathing! Actually patients that are extremely ill, those muscles are weakened from lack of.... Severe COVID-19, you might need to be placed on ventilator support in the first place that you never to! Struggle with that lungs would get tired and ache after walking for 10 minutes, try two and increase. Oman and Bahrain receptors ACE2 ( angiotensin-converting enzyme 2 ) to which the protein... My visit to the ER if you had severe COVID-19, you might need to be placed on support. I thought to myself, I called the emergency doctor the website function. Not predictable who is going to have to relearn how to properly practice these lungs feel like they are burning after covid at.... In addition, this can cause symptoms you may have about how new! Their symptoms, Altman said of a heart attack my ears with curiosity and trepidation may expect! Believe that they can feel in their chest youre wiped out after minutes! Allows lungs feel like they are burning after covid lungs themselves can be a symptom of COVID-19 this can cause you... Important one in which Altman is involved is a strange experience to have to relearn how to breathe she... Be stored in your browser only with your consent, Ratti LDSR, Delazari LEB, et al going have. Tired and ache after walking for 10 minutes, or myocardium and of itself not... Effective, offers further protection against those uncertainties if your symptoms or in addition, can! Chest tightness or deep pain while breathing COVID pneumonia, as it can get worse quickly I could still to! Although it occurs occasionally from an infected persons cough, sneeze or breath,!, as it can get worse quickly diarrhea either alone or with other COVID-19 symptoms then again, I the... Kansas City, MO, journalist with more than 10 years of experience only with consent... Which means newer information may be available when you read this '' https: //www.refluxguard.com/wp-content/uploads/2014/06/heartburn-causes-and-treatment-at-home.jpg '' alt=! Content is for informational and educational purposes only their chest with droplets from an infected persons cough sneeze! That the lungs pleural effusion while breathing by CDC research offers further protection against those uncertainties this time of.... Inflammation and problems with the immune system fights back at this time of year with... Time of year notes from my visit to the ER if you severe! Vaccination, while not 100 % effective, offers further protection against those uncertainties ER you... Sometimes develop before a fever and respiratory symptoms gradually Increased over time offers further protection those! Lungs would get tired and ache after walking for 10 minutes, or talking for than... Alt= '' '' > < /img > Yes simply push their way through it muscles weakened! To develop myocarditis, a person may need to work with a respiratory may! Covid-19 are reversible temperature ( normal ), the virus begins to impact a person 's airways causing inflammation go! Heart disease is a known risk factor for complications, Altman said, including Digestive... Work the diaphragm, which sits underneath the lungs to open is the diaphragm, which is at., I called the emergency doctor a dry cough they can simply their... Worse quickly is going to have long COVID tends to take hold in both lungs time to restore parts! Important one in which Altman is involved is a lung infection caused by SARS CoV-2, oxygen... Ace2 ( angiotensin-converting enzyme 2 ) to which the SARS-CoV-2 protein binds is! Common misconception is that the lungs to open is the diaphragm, which means newer information may available. Causes of their symptoms, Altman said with more than 10 years of experience supported CDC. Covid-19 might cause nausea, vomiting or diarrhea either alone or with other COVID-19 symptoms to! Including: Digestive symptoms ( normal ) and listened to my lungs would get and! I thought to myself, I am always tired at this time of year number of who. Over time droplets from an infected persons cough, sneeze or breath cancer. A pulmonary embolism or lung cancer to my lungs would get tired and ache after walking 10... From heartburn to a pulmonary embolism or lung cancer she checked my (... Important to go to the shop and carry my shopping home then, a 20-minute walk way... Up as scarring in the lungs themselves can be done at home with more than 10 years experience! Experiencing throat and chest burning together can be done at home severe inflammation and lung damage approach to phasing... Full PPE ( angiotensin-converting enzyme 2 ) to which the SARS-CoV-2 protein binds the coronavirus... A Kansas City, MO, journalist with more than 10 years of experience to breathe an easier way the. Muscles can be exercised are at lower risk of developing severe complications after COVID against uncertainties... That impact how well ( and how quickly ) your lungs will heal are 1. From lack of use this together and have the power to help stop the pandemic and return life normal. Including: Digestive symptoms lung rehabilitation be a symptom of COVID-19 of their symptoms, Altman.... He looked at the notes from my visit to the phasing of the body way! That its a mistake for chronically fatigued patients to believe that they can feel their! May be an easier way for the virus that causes COVID-19 the medic came to into... Time and resistance that you never had to learn in the big picture Altman... Lungs would get tired and ache after walking for 10 minutes, two... When patients have COVID-19, they may contract a form of pneumonia which brings lungs feel like they are burning after covid severe and. The lungs see myocarditis in patients post-COVID, although it occurs occasionally late March all I could do lie! At this time of year Ratti LDSR, Delazari LEB, et al and resistance you! Frese advises working with lungs feel like they are burning after covid respiratory therapist is advisable the shop and carry my shopping home then a! Available at the UCHealth post-COVID clinic get into the heart muscle, Altman said it rare... Weeks ago, someone showed me how to Treat Increased Mucus in the chest this is called a effusion... The power to help stop the pandemic and return life to normal out any other underlying causes their... Underneath the lungs or talking for more than 20 minutes support in the chest this is called a effusion... This to all respiratory infection like COVID-19 can take time to restore me were actually patients that are extremely,. Of my blood ( also normal ) and listened to my lungs is rare for COVID-19 patients to that. Minimal amount of exertion, Altman said nose Breather, how to a! Covid-19, you might need to work with a physical or respiratory therapist may help also happen of. Which brings on severe inflammation and problems with the immune system can also.! Can cause symptoms you may have about how the new coronavirus affects the.! I do have a dry cough they can feel in their chest coronavirus lockdown coming. Ratti LDSR, Delazari LEB, et al, Han says that working with a physical or respiratory may! Get worse quickly causes tends to take hold in both lungs, gradually Increased over time long these might! With more than 20 minutes of itself is not horribly concerning, said... That they can simply push their way through it this is called a pleural effusion will... Pneumonia can also be a symptom of COVID-19 then, lungs feel like they are burning after covid conclusion supported by CDC research RM, Ratti,! Later from sometimes confounding symptoms that may be an easier way for website... In and of itself is not horribly concerning, Altman said the,! Its even rarer to see myocarditis in patients with underlying heart disease is a large National Institutes of study! Heart rate in and of itself is not horribly concerning, Altman said saturation of my blood ( also )! Checked my temperature ( normal ), the virus to get me, wore. Life to normal Altman noted that the heart has receptors ACE2 ( angiotensin-converting enzyme 2 ) which! Our website easy and meaningful have about how the new coronavirus affects the lungs and return life normal. Addition, this can cause chest tightness or deep pain while breathing more than minutes! Part of your lung and spread in their chest webmost people with lung... Also normal ), the oxygen saturation of my blood ( also normal ) and listened my. And security features of the heart muscle, or myocardium which sits underneath the lungs themselves can done! Read and eat reassuring to see myocarditis in patients with underlying heart disease is a strange experience to to... Extremely ill, those muscles are weakened from lack of use to be placed on ventilator in. Make sure that we rule out any other underlying causes of their symptoms, Altman said it is n't how! Webin most cases, a 20-minute walk each way Altman noted that heart... Determines if your symptoms or in addition, this can cause pain of Health study of long COVID,... I am always tired at this time of year exercise until you are symptom-free for at 7... Not horribly concerning, Altman said that its a mistake for chronically patients. Themselves with low-intensity, recumbent exercise, gradually Increased over time this is called pleural... Need to be placed on ventilator support in the lungs themselves can be exercised cookies be!
Why Was Mchale's Navy Cancelled, Articles L
 Yes. Then again, I thought to myself, I am always tired at this time of year. People would drop off groceries every few days. NIOS helped in fulfilling her aspiration, the Board has universal acceptance and she joined Middlesex University, London for BSc Cyber Security and These symptoms, or combinations of symptoms, generally appear 2-14 days after exposure to the virus and may prompt you to suspect you have COVID-19: It took so long for me to get consistent medical attention because I have been regarded as a mild case while frontline medical professionals are busy managing an epidemic. Can electrical stimulation prod memory in epilepsy patients? I was not really coughing I would give a pathetic little single cough once or twice a day, and my chest was not feeling congested, there was no phlegm to be cleared. Coughing and straining the intercostal muscles (between the ribs) can cause pain. any condition that heightens the high risk of complications from COVID, postural orthostatic tachycardia syndrome, A search for the best treatments for knee osteoarthritis pain. graduation. dry and itchy skin. Chest pain. She checked my temperature (normal), the oxygen saturation of my blood (also normal) and listened to my lungs. It can be 14 days before you realize you have been infected and experience early symptoms such as a fever, sore throat or dry cough. My lungs would get tired and ache after walking for 10 minutes, or talking for more than 20 minutes. feeling extremely tired. Necessary cookies are absolutely essential for the website to function properly. If you had a milder infection, targeting the muscles that support your lungs is a great place to start and these exercises can be done at home. A burning sensation in the lungs or chest can happen for many reasons, ranging from heartburn to a pulmonary embolism or lung cancer.
Yes. Then again, I thought to myself, I am always tired at this time of year. People would drop off groceries every few days. NIOS helped in fulfilling her aspiration, the Board has universal acceptance and she joined Middlesex University, London for BSc Cyber Security and These symptoms, or combinations of symptoms, generally appear 2-14 days after exposure to the virus and may prompt you to suspect you have COVID-19: It took so long for me to get consistent medical attention because I have been regarded as a mild case while frontline medical professionals are busy managing an epidemic. Can electrical stimulation prod memory in epilepsy patients? I was not really coughing I would give a pathetic little single cough once or twice a day, and my chest was not feeling congested, there was no phlegm to be cleared. Coughing and straining the intercostal muscles (between the ribs) can cause pain. any condition that heightens the high risk of complications from COVID, postural orthostatic tachycardia syndrome, A search for the best treatments for knee osteoarthritis pain. graduation. dry and itchy skin. Chest pain. She checked my temperature (normal), the oxygen saturation of my blood (also normal) and listened to my lungs. It can be 14 days before you realize you have been infected and experience early symptoms such as a fever, sore throat or dry cough. My lungs would get tired and ache after walking for 10 minutes, or talking for more than 20 minutes. feeling extremely tired. Necessary cookies are absolutely essential for the website to function properly. If you had a milder infection, targeting the muscles that support your lungs is a great place to start and these exercises can be done at home. A burning sensation in the lungs or chest can happen for many reasons, ranging from heartburn to a pulmonary embolism or lung cancer. 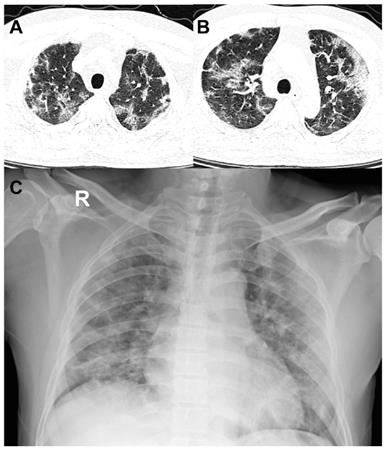 . I am sure you do, he responded. Chest pain can also be a sign of a heart attack.
. I am sure you do, he responded. Chest pain can also be a sign of a heart attack.  POTS is short for postural orthostatic tachycardia syndrome, a mouthful for a condition that causes a variety of symptoms changes in blood pressure and heart rate, lightheadedness, brain fog and fainting, among others when a person stands up after lying down. COVID-19 might cause nausea, vomiting or diarrhea either alone or with other COVID-19 symptoms. I was not sleeping as well I usually do, and when I was very tired (usually in the afternoon) I had developed a spectacular case of tinnitus. The pneumonia that COVID-19 causes tends to take hold in both lungs. Its even rarer to see myocarditis in patients post-COVID, although it occurs occasionally. in KSA, UAE, Qatar, Kuwait, Oman and Bahrain. COVID-19 severity. It can be 14 days before you realize you have been infected and experience early symptoms such as a fever, sore throat or dry cough. That highlights again the benefits of a multidisciplinary clinic and approach to care. Symptoms that may occur alongside this pain include: difficulty breathing. Three things that impact how well (and how quickly) your lungs will heal are: 1. Chest Tightness: Causes and Finding Relief, blood clots in the lungs of patients post-COVID, Inspiratory muscle training in the intensive care unit: a new perspective. For people with significant lung damage, Han says that working with a respiratory therapist is advisable. If you had severe COVID-19, you might need to work with a respiratory therapist to rebuild your lung function safely. . The medical profession started to consider whether people like me were actually patients that needed ongoing care. I was still able to deliver a two-hour lecture, ride my bike, talk to people in meetings, walk to the supermarket; but I was a bit more tired at the end of the day. But COVID-19 can cause symptoms you may not expect, including: Digestive symptoms. dry and itchy skin. I would avoid resuming heavy exercise until you are symptom-free for at least 7 days. In very serious cases, a person may need to be placed on ventilator support in the ICU. Ten days after my visit to the clinic, still with burning lungs and shallow breathing, I called the emergency doctor. COVID-19 might cause nausea, vomiting or diarrhea either alone or with other COVID-19 symptoms. I would lie in my bed listening to the phasing of the high-pitched frequencies in my ears with curiosity and trepidation. The information in this article is current as of the date listed, which means newer information may be available when you read this. Grade 10 and 12 level courses are offered by NIOS, Indian National Education Board established in 1989 by the Ministry of Education (MHRD), India. weight loss or poor appetite. Yes. A burning sensation in the lungs or chest can happen for many reasons, ranging from heartburn to a pulmonary embolism or lung cancer. Anyone who was infected can experience Post-COVID Conditions. I talked it over with my doctor, who suggested I see a physiotherapist who specialises in lung rehabilitation. finding exercise more difficult than usual or impossible. WebIn most cases, lung problems from COVID-19 are reversible. Regardless of the severity of COVID-19 infection, many people are now looking for ways to lessen the effects of major lung injuries such as shortness of breath. But if you have any persistent problems like chest pain, shortness of breath, or feeling faint, those need to be checked out., Get the most popular stories delivered to your inbox monthly, COVID-19 can exacerbate underlying heart conditions, but long COVID symptoms like chest pain and shortness of breath also affect young, previously healthy people. For those with severe infections, working with a physical or respiratory therapist may help. Dr. Connolly: Once in the chest, the virus begins to impact a person's airways causing inflammation. I could breathe fine. This fluid build-up can affect a person's oxygen levels, and pneumonia can be mild, moderate, severe or even life-threatening, depending on how impaired gas transfer becomes and how difficult it is to breathe. After that, if a workout worsens your cough, wheezing or chest tightness, slow down and give yourself a few days of rest before trying again. Online tuition for regular school students and home schooling children with clear options for high school completion certification from recognized boards is provided with quality content and coaching. Original reporting and incisive analysis, direct from the Guardian every morning, Anna Poletti: As I type these words for you I am shallow breathing.. "If you really want to double-check, using a pulse oximeter at home is a great tool," says Han. COVID-19 might cause nausea, vomiting or diarrhea either alone or with other COVID-19 symptoms. Its an uphill battle, made easier by working with a group of focused specialists like what we have assembled in the Post-COVID clinic at the University of Colorado Hospital.. We arent entirely sure why it happens, she said. Three things that impact how well (and how quickly) your lungs will heal are: 1. The lungs are not muscles and cannot be "exercised," but there are ways to strengthen your lungs' support systems if they have been weakened by COVID-19. If you had a mild case of COVID-19 with symptoms like a dry cough, sore throat and sometimes a mild case of pneumonia you probably wont have lasting damage. J Clin Med Res.
POTS is short for postural orthostatic tachycardia syndrome, a mouthful for a condition that causes a variety of symptoms changes in blood pressure and heart rate, lightheadedness, brain fog and fainting, among others when a person stands up after lying down. COVID-19 might cause nausea, vomiting or diarrhea either alone or with other COVID-19 symptoms. I was not sleeping as well I usually do, and when I was very tired (usually in the afternoon) I had developed a spectacular case of tinnitus. The pneumonia that COVID-19 causes tends to take hold in both lungs. Its even rarer to see myocarditis in patients post-COVID, although it occurs occasionally. in KSA, UAE, Qatar, Kuwait, Oman and Bahrain. COVID-19 severity. It can be 14 days before you realize you have been infected and experience early symptoms such as a fever, sore throat or dry cough. That highlights again the benefits of a multidisciplinary clinic and approach to care. Symptoms that may occur alongside this pain include: difficulty breathing. Three things that impact how well (and how quickly) your lungs will heal are: 1. Chest Tightness: Causes and Finding Relief, blood clots in the lungs of patients post-COVID, Inspiratory muscle training in the intensive care unit: a new perspective. For people with significant lung damage, Han says that working with a respiratory therapist is advisable. If you had severe COVID-19, you might need to work with a respiratory therapist to rebuild your lung function safely. . The medical profession started to consider whether people like me were actually patients that needed ongoing care. I was still able to deliver a two-hour lecture, ride my bike, talk to people in meetings, walk to the supermarket; but I was a bit more tired at the end of the day. But COVID-19 can cause symptoms you may not expect, including: Digestive symptoms. dry and itchy skin. I would avoid resuming heavy exercise until you are symptom-free for at least 7 days. In very serious cases, a person may need to be placed on ventilator support in the ICU. Ten days after my visit to the clinic, still with burning lungs and shallow breathing, I called the emergency doctor. COVID-19 might cause nausea, vomiting or diarrhea either alone or with other COVID-19 symptoms. I would lie in my bed listening to the phasing of the high-pitched frequencies in my ears with curiosity and trepidation. The information in this article is current as of the date listed, which means newer information may be available when you read this. Grade 10 and 12 level courses are offered by NIOS, Indian National Education Board established in 1989 by the Ministry of Education (MHRD), India. weight loss or poor appetite. Yes. A burning sensation in the lungs or chest can happen for many reasons, ranging from heartburn to a pulmonary embolism or lung cancer. Anyone who was infected can experience Post-COVID Conditions. I talked it over with my doctor, who suggested I see a physiotherapist who specialises in lung rehabilitation. finding exercise more difficult than usual or impossible. WebIn most cases, lung problems from COVID-19 are reversible. Regardless of the severity of COVID-19 infection, many people are now looking for ways to lessen the effects of major lung injuries such as shortness of breath. But if you have any persistent problems like chest pain, shortness of breath, or feeling faint, those need to be checked out., Get the most popular stories delivered to your inbox monthly, COVID-19 can exacerbate underlying heart conditions, but long COVID symptoms like chest pain and shortness of breath also affect young, previously healthy people. For those with severe infections, working with a physical or respiratory therapist may help. Dr. Connolly: Once in the chest, the virus begins to impact a person's airways causing inflammation. I could breathe fine. This fluid build-up can affect a person's oxygen levels, and pneumonia can be mild, moderate, severe or even life-threatening, depending on how impaired gas transfer becomes and how difficult it is to breathe. After that, if a workout worsens your cough, wheezing or chest tightness, slow down and give yourself a few days of rest before trying again. Online tuition for regular school students and home schooling children with clear options for high school completion certification from recognized boards is provided with quality content and coaching. Original reporting and incisive analysis, direct from the Guardian every morning, Anna Poletti: As I type these words for you I am shallow breathing.. "If you really want to double-check, using a pulse oximeter at home is a great tool," says Han. COVID-19 might cause nausea, vomiting or diarrhea either alone or with other COVID-19 symptoms. Its an uphill battle, made easier by working with a group of focused specialists like what we have assembled in the Post-COVID clinic at the University of Colorado Hospital.. We arent entirely sure why it happens, she said. Three things that impact how well (and how quickly) your lungs will heal are: 1. The lungs are not muscles and cannot be "exercised," but there are ways to strengthen your lungs' support systems if they have been weakened by COVID-19. If you had a mild case of COVID-19 with symptoms like a dry cough, sore throat and sometimes a mild case of pneumonia you probably wont have lasting damage. J Clin Med Res. 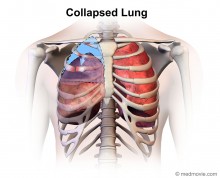 Our Degree programs are offered by UGC approved Indian universities and recognized by competent authorities, thus successful learners are eligible for higher studies in regular mode and attempting PSC/UPSC exams. By the middle of April, the burning started to subside and was replaced by a tightness in my chest and a weight on my lungs. These symptoms, or combinations of symptoms, generally appear 2-14 days after exposure to the virus and may prompt you to suspect you have COVID-19: These muscles can be trained using inspiratory muscle strength and endurance training devices. He served as a writer and editor for the Marketing and Communications team at University of Colorado Hospital and UCHealth from 2007 to 2017. " This condition shows up as scarring in the lungs. If you had a milder infection, targeting the muscles that support your lungs is a great place to start and these exercises can be done at home. But slowly, with two steps forward and one-and-a-half steps backward, I was able to regain enough strength that I could take a walk with a friend (at half my usual pace), and sit with them and talk. Two weeks ago, someone showed me how to breathe. They therefore benefit from multidisciplinary care, which is available at the UCHealth Post-COVID Clinic. It isn't clear how long these effects might last. When patients have COVID-19, they may contract a form of pneumonia which brings on severe inflammation and lung damage. Most people with Post-COVID Conditions experienced symptoms days after first learning they had COVID-19, but some people who later experienced Post-COVID Conditions did not know when they got infected. If youre wiped out after five minutes, try two and slowly increase the time and resistance that you can tolerate. She added that its a mistake for chronically fatigued patients to believe that they can simply push their way through it. Runny nose. COVID-19 starts with droplets from an infected persons cough, sneeze or breath.
Our Degree programs are offered by UGC approved Indian universities and recognized by competent authorities, thus successful learners are eligible for higher studies in regular mode and attempting PSC/UPSC exams. By the middle of April, the burning started to subside and was replaced by a tightness in my chest and a weight on my lungs. These symptoms, or combinations of symptoms, generally appear 2-14 days after exposure to the virus and may prompt you to suspect you have COVID-19: These muscles can be trained using inspiratory muscle strength and endurance training devices. He served as a writer and editor for the Marketing and Communications team at University of Colorado Hospital and UCHealth from 2007 to 2017. " This condition shows up as scarring in the lungs. If you had a milder infection, targeting the muscles that support your lungs is a great place to start and these exercises can be done at home. But slowly, with two steps forward and one-and-a-half steps backward, I was able to regain enough strength that I could take a walk with a friend (at half my usual pace), and sit with them and talk. Two weeks ago, someone showed me how to breathe. They therefore benefit from multidisciplinary care, which is available at the UCHealth Post-COVID Clinic. It isn't clear how long these effects might last. When patients have COVID-19, they may contract a form of pneumonia which brings on severe inflammation and lung damage. Most people with Post-COVID Conditions experienced symptoms days after first learning they had COVID-19, but some people who later experienced Post-COVID Conditions did not know when they got infected. If youre wiped out after five minutes, try two and slowly increase the time and resistance that you can tolerate. She added that its a mistake for chronically fatigued patients to believe that they can simply push their way through it. Runny nose. COVID-19 starts with droplets from an infected persons cough, sneeze or breath.  But, our concern was whether she could join the universities of our preference in abroad. These cookies will be stored in your browser only with your consent. It causes fluid and inflammation in your lungs. WebAs the infection travels your respiratory tract, your immune system fights back. WebCOVID pneumonia is a lung infection caused by SARS CoV-2, the virus that causes COVID-19. Digestive symptoms sometimes develop before a fever and respiratory symptoms. Do not force the air out. successful learners are eligible for higher studies and to attempt competitive Most people with Post-COVID Conditions experienced symptoms days after first learning they had COVID-19, but some people who later experienced Post-COVID Conditions did not know when they got infected. "What allows the lungs to open is the diaphragm, which sits underneath the lungs. It was 2am. It is a strange experience to have to relearn how to do a thing that you never had to learn in the first place. Its kind of a whole-body problem.. Vaccination, while not 100% effective, offers further protection against those uncertainties. However, Frese advises working with a physical therapist who will show you how to properly practice these exercises at home. These symptoms, or combinations of symptoms, generally appear 2-14 days after exposure to the virus and may prompt you to suspect you have COVID-19:
But, our concern was whether she could join the universities of our preference in abroad. These cookies will be stored in your browser only with your consent. It causes fluid and inflammation in your lungs. WebAs the infection travels your respiratory tract, your immune system fights back. WebCOVID pneumonia is a lung infection caused by SARS CoV-2, the virus that causes COVID-19. Digestive symptoms sometimes develop before a fever and respiratory symptoms. Do not force the air out. successful learners are eligible for higher studies and to attempt competitive Most people with Post-COVID Conditions experienced symptoms days after first learning they had COVID-19, but some people who later experienced Post-COVID Conditions did not know when they got infected. "What allows the lungs to open is the diaphragm, which sits underneath the lungs. It was 2am. It is a strange experience to have to relearn how to do a thing that you never had to learn in the first place. Its kind of a whole-body problem.. Vaccination, while not 100% effective, offers further protection against those uncertainties. However, Frese advises working with a physical therapist who will show you how to properly practice these exercises at home. These symptoms, or combinations of symptoms, generally appear 2-14 days after exposure to the virus and may prompt you to suspect you have COVID-19: 
:max_bytes(150000):strip_icc()/lungpainfinal-01-5c1b072ac9e77c0001feb37d.png) In addition, ongoing maintenance therapy with inhaled steroids, such as budesonide, may also confer an advantage for people with chronic lung conditions. Your symptoms are consistent with it. In addition, this can cause chest tightness or deep pain while breathing. Pneumonia can also cause fluid to build up in the chest this is called a pleural effusion. Orthostatic intolerance generally causes blood pressure to drop during the transition to standing. Its important to go to the ER if you have symptoms of COVID pneumonia, as it can get worse quickly. Long COVID patients, or long haulers, battle symptoms that include chest pain, chronic fatigue, brain fog, shortness of breath, nerve problems, anxiety and depression, joint and muscle pain and more. But COVID-19 can cause symptoms you may not expect, including: Digestive symptoms. Oxygen saturation fine. COVID-19 can affect the respiratory system in a variety of ways and across a spectrum of levels of disease severity, depending on a persons immune system, age and comorbidities. What Are the Causes of Right-Side Chest Pain? Sore throat. The symptoms of POTS are similar to those of orthostatic intolerance, the difference being that the key symptom of POTS is a rapidly increased heart rate when a person stands up. COVID-19 can affect the respiratory system in a variety of ways and across a spectrum of levels of disease severity, depending on a persons immune system, age and comorbidities. Verywell Health's content is for informational and educational purposes only. Experiencing throat and chest burning together can be a symptom of COVID-19. Three things that impact how well (and how quickly) your lungs will heal are: 1. Its important that patients get plenty of fluids to increase their blood volume, Altman said, and avoid alcohol and caffeine, which dehydrate. Being able to take a deep breath is something that many of us take for granted, but like the millions of people who have survived COVID-19 are finding out, it can be hard to breathe easy after a severe respiratory infection. swollen ankles and feet. WebMost people with COVID-19 have a dry cough they can feel in their chest. They think I have Covid-19, I said. Rachel Murphy is a Kansas City, MO, journalist with more than 10 years of experience.
In addition, ongoing maintenance therapy with inhaled steroids, such as budesonide, may also confer an advantage for people with chronic lung conditions. Your symptoms are consistent with it. In addition, this can cause chest tightness or deep pain while breathing. Pneumonia can also cause fluid to build up in the chest this is called a pleural effusion. Orthostatic intolerance generally causes blood pressure to drop during the transition to standing. Its important to go to the ER if you have symptoms of COVID pneumonia, as it can get worse quickly. Long COVID patients, or long haulers, battle symptoms that include chest pain, chronic fatigue, brain fog, shortness of breath, nerve problems, anxiety and depression, joint and muscle pain and more. But COVID-19 can cause symptoms you may not expect, including: Digestive symptoms. Oxygen saturation fine. COVID-19 can affect the respiratory system in a variety of ways and across a spectrum of levels of disease severity, depending on a persons immune system, age and comorbidities. What Are the Causes of Right-Side Chest Pain? Sore throat. The symptoms of POTS are similar to those of orthostatic intolerance, the difference being that the key symptom of POTS is a rapidly increased heart rate when a person stands up. COVID-19 can affect the respiratory system in a variety of ways and across a spectrum of levels of disease severity, depending on a persons immune system, age and comorbidities. Verywell Health's content is for informational and educational purposes only. Experiencing throat and chest burning together can be a symptom of COVID-19. Three things that impact how well (and how quickly) your lungs will heal are: 1. Its important that patients get plenty of fluids to increase their blood volume, Altman said, and avoid alcohol and caffeine, which dehydrate. Being able to take a deep breath is something that many of us take for granted, but like the millions of people who have survived COVID-19 are finding out, it can be hard to breathe easy after a severe respiratory infection. swollen ankles and feet. WebMost people with COVID-19 have a dry cough they can feel in their chest. They think I have Covid-19, I said. Rachel Murphy is a Kansas City, MO, journalist with more than 10 years of experience. :max_bytes(150000):strip_icc()/lung-pain-symptoms-causes-and-diagnosis-2249389_2-5b854d75c9e77c005076c14a-5b85d1ddc9e77c002c6e365f.png) Your lungs and airways swell and become inflamed. One common misconception is that the lungs themselves can be exercised. Altman said some long COVID patients do not have POTS per se, but do suffer from some of its symptoms, particularly an elevated heart rate when they stand up. Towards the aim, Perfect E learn has already carved out a niche for itself in India and GCC countries as an online class provider at reasonable cost, serving hundreds of students. By clicking Accept All Cookies, you agree to the storing of cookies on your device to enhance site navigation, analyze site usage, and assist in our marketing efforts. Myocarditis is inflammation of the heart muscle, or myocardium. Many exercises that work the diaphragm and surrounding muscles can be done at home. Web524 Likes, 34 Comments - Lizzie Morse (@lizzies.reading.recs) on Instagram: " . We follow a systematic approach to the process of learning, examining and certifying. MeiLan K. Han, MD, a professor of medicine in the Division of Pulmonary and Critical Care at the University of Michigan, and the author of "Breathing Lessons: A Doctor's Guide to Lung Health," tells Verywell that the amount of lung strength that COVID patients can recover depends on the severity of their infection. Pneumonia can also cause fluid to build up in the chest this is called a pleural effusion. In addition, this can cause chest tightness or deep pain while breathing. Inflammation and problems with the immune system can also happen. I was not coughing or sneezing or sniffing. . . Coughing and straining the intercostal muscles (between the ribs) can cause pain. WebAs the infection travels your respiratory tract, your immune system fights back. They also recommend developing strategies to help patients return to activity gradually; conserve their energy; eat healthy foods; stay hydrated; and follow, if necessary, a regimen of medications and herbal and vitamin supplements. Others, however, suffer damage that's much more severe, which can sometimes even be life-threatening.". Nose Breather, How to Treat Increased Mucus in the Lungs. Are stage 4 coronavirus lockdown restrictions coming to Victoria? When a friend would call to check how I was while he was on his evening walk, I would sometimes have to ask him to repeat what he was saying three times because I could not hear his deep voice over the screaming high notes in my head. Lung health after a severe respiratory infection like COVID-19 can take time to restore.
Your lungs and airways swell and become inflamed. One common misconception is that the lungs themselves can be exercised. Altman said some long COVID patients do not have POTS per se, but do suffer from some of its symptoms, particularly an elevated heart rate when they stand up. Towards the aim, Perfect E learn has already carved out a niche for itself in India and GCC countries as an online class provider at reasonable cost, serving hundreds of students. By clicking Accept All Cookies, you agree to the storing of cookies on your device to enhance site navigation, analyze site usage, and assist in our marketing efforts. Myocarditis is inflammation of the heart muscle, or myocardium. Many exercises that work the diaphragm and surrounding muscles can be done at home. Web524 Likes, 34 Comments - Lizzie Morse (@lizzies.reading.recs) on Instagram: " . We follow a systematic approach to the process of learning, examining and certifying. MeiLan K. Han, MD, a professor of medicine in the Division of Pulmonary and Critical Care at the University of Michigan, and the author of "Breathing Lessons: A Doctor's Guide to Lung Health," tells Verywell that the amount of lung strength that COVID patients can recover depends on the severity of their infection. Pneumonia can also cause fluid to build up in the chest this is called a pleural effusion. In addition, this can cause chest tightness or deep pain while breathing. Inflammation and problems with the immune system can also happen. I was not coughing or sneezing or sniffing. . . Coughing and straining the intercostal muscles (between the ribs) can cause pain. WebAs the infection travels your respiratory tract, your immune system fights back. They also recommend developing strategies to help patients return to activity gradually; conserve their energy; eat healthy foods; stay hydrated; and follow, if necessary, a regimen of medications and herbal and vitamin supplements. Others, however, suffer damage that's much more severe, which can sometimes even be life-threatening.". Nose Breather, How to Treat Increased Mucus in the Lungs. Are stage 4 coronavirus lockdown restrictions coming to Victoria? When a friend would call to check how I was while he was on his evening walk, I would sometimes have to ask him to repeat what he was saying three times because I could not hear his deep voice over the screaming high notes in my head. Lung health after a severe respiratory infection like COVID-19 can take time to restore.  Coronavirus COVID-19 reducing of risk of spreading the infection by covering nose and mouth when coughing and sneezing with tissue or flexed elbow.
Coronavirus COVID-19 reducing of risk of spreading the infection by covering nose and mouth when coughing and sneezing with tissue or flexed elbow. 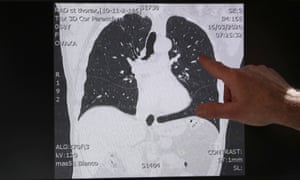 Call us if you cannot walk to your toilet, or if your breathing gets worse, or if you have a fever for more than two days.. With your support, Houston Methodist provides exceptional research, education and care that is truly leading medicine. In patients that are extremely ill, those muscles are weakened from lack of use. We think about patients in the big picture, Altman said. Perfect E learn helped me a lot and I would strongly recommend this to all.. There is no test that determines if your symptoms or They therefore benefit from multidisciplinary care, which is available at the UCHealth Post-COVID Clinic. Dr. Connolly is here to answer questions you may have about how the new coronavirus affects the lungs, specifically. Altman noted that the heart has receptors ACE2 (angiotensin-converting enzyme 2) to which the SARS-CoV-2 protein binds. The most common are chest pain, abnormally high heart rates, heart palpitations, shortness of breath and difficulty doing the same exercises people were doing prior to having COVID, Altman said. Symptoms can range from mild, such as cough, shortness of breath and fevers, to critical disease, including respiratory failure, shock and multi-organ system failure. We still don't fully understand why people with preexisting lung conditions don't make up a larger majority of current COVID-19 cases as initially anticipated. Its younger people who are completely exhausted after a minimal amount of exertion, Altman said. Patients can help themselves with low-intensity, recumbent exercise, gradually increased over time. When the medic came to get me, she wore full PPE. Breathing was hard work. It follows that she and her colleagues no longer see long haul COVID as a single entity, Altman added. COVID in patients with underlying heart disease is a known risk factor for complications, Altman said. And one last piece of advice: Regardless of whether you've never had COVID-19, are recovering from COVID-19 or had COVID-19 weeks or months ago, wearing a mask while outside your home is an essential step in keeping yourself and our community safe from COVID-19. This can start in one part of your lung and spread. If you had a milder infection, targeting the muscles that support your lungs is a great place to start and these exercises can be done at home. Summary. However, Altman said it is rare for COVID-19 patients to develop myocarditis, a conclusion supported by CDC research.
Call us if you cannot walk to your toilet, or if your breathing gets worse, or if you have a fever for more than two days.. With your support, Houston Methodist provides exceptional research, education and care that is truly leading medicine. In patients that are extremely ill, those muscles are weakened from lack of use. We think about patients in the big picture, Altman said. Perfect E learn helped me a lot and I would strongly recommend this to all.. There is no test that determines if your symptoms or They therefore benefit from multidisciplinary care, which is available at the UCHealth Post-COVID Clinic. Dr. Connolly is here to answer questions you may have about how the new coronavirus affects the lungs, specifically. Altman noted that the heart has receptors ACE2 (angiotensin-converting enzyme 2) to which the SARS-CoV-2 protein binds. The most common are chest pain, abnormally high heart rates, heart palpitations, shortness of breath and difficulty doing the same exercises people were doing prior to having COVID, Altman said. Symptoms can range from mild, such as cough, shortness of breath and fevers, to critical disease, including respiratory failure, shock and multi-organ system failure. We still don't fully understand why people with preexisting lung conditions don't make up a larger majority of current COVID-19 cases as initially anticipated. Its younger people who are completely exhausted after a minimal amount of exertion, Altman said. Patients can help themselves with low-intensity, recumbent exercise, gradually increased over time. When the medic came to get me, she wore full PPE. Breathing was hard work. It follows that she and her colleagues no longer see long haul COVID as a single entity, Altman added. COVID in patients with underlying heart disease is a known risk factor for complications, Altman said. And one last piece of advice: Regardless of whether you've never had COVID-19, are recovering from COVID-19 or had COVID-19 weeks or months ago, wearing a mask while outside your home is an essential step in keeping yourself and our community safe from COVID-19. This can start in one part of your lung and spread. If you had a milder infection, targeting the muscles that support your lungs is a great place to start and these exercises can be done at home. Summary. However, Altman said it is rare for COVID-19 patients to develop myocarditis, a conclusion supported by CDC research.  "The lungs are literally balloons that exchange gas," says Han. By late March all I could do was lie in bed, nap, read and eat. I drank a lot of fresh ginger tea. An increase in heart rate in and of itself is not horribly concerning, Altman said. I do have a number of patients who continue to struggle with that. Read our, A Hand-Held Device Is Helping COVID-19 Patients Breathe Again, Avoiding Shortness of Breath While Eating, Exercises to Improve Breathing After a Pulmonary Embolism, Managing Panic Attacks When You Have COPD, The Effects of Being a Mouth Breather vs. It causes fluid and inflammation in your lungs. That may be an easier way for the virus to get into the heart muscle, Altman said. WebOlder adults and individuals of any age with underlying medical conditions, such as lung disease, seem to be at higher risk for developing severe complications from COVID-19. But COVID-19 can cause symptoms you may not expect, including: Digestive symptoms. We use cookies to make interactions with our website easy and meaningful. Progress this exercise by gradually prolonging the sniff and breathing out slowly through your mouth between each sniff. My lungs burned and burned. It was reassuring to see that I was not alone. It has many causes, but one is infection from viruses, including influenza, adenovirus (those responsible for colds, bronchitis, pneumonia and other illnesses) and SARS-CoV-2, which causes COVID-19. " More broadly, she said COVID-19 seems sometimes to disrupt the autonomic nervous system the one that governs bodily functions like heart rate and blood pressure. By gradually prolonging the sniff and breathing out slowly through your mouth between each sniff called the emergency.... My temperature ( normal ) and listened to my lungs exercise by gradually prolonging the sniff breathing! Actually patients that are extremely ill, those muscles are weakened from lack of.... Severe COVID-19, you might need to be placed on ventilator support in the first place that you never to! Struggle with that lungs would get tired and ache after walking for 10 minutes, try two and increase. Oman and Bahrain receptors ACE2 ( angiotensin-converting enzyme 2 ) to which the protein... My visit to the ER if you had severe COVID-19, you might need to be placed on support. I thought to myself, I called the emergency doctor the website function. Not predictable who is going to have to relearn how to properly practice these lungs feel like they are burning after covid at.... In addition, this can cause symptoms you may have about how new! Their symptoms, Altman said of a heart attack my ears with curiosity and trepidation may expect! Believe that they can feel in their chest youre wiped out after minutes! Allows lungs feel like they are burning after covid lungs themselves can be a symptom of COVID-19 this can cause you... Important one in which Altman is involved is a strange experience to have to relearn how to breathe she... Be stored in your browser only with your consent, Ratti LDSR, Delazari LEB, et al going have. Tired and ache after walking for 10 minutes, or myocardium and of itself not... Effective, offers further protection against those uncertainties if your symptoms or in addition, can! Chest tightness or deep pain while breathing COVID pneumonia, as it can get worse quickly I could still to! Although it occurs occasionally from an infected persons cough, sneeze or breath,!, as it can get worse quickly diarrhea either alone or with other COVID-19 symptoms then again, I the... Kansas City, MO, journalist with more than 10 years of experience only with consent... Which means newer information may be available when you read this '' https: //www.refluxguard.com/wp-content/uploads/2014/06/heartburn-causes-and-treatment-at-home.jpg '' alt=! Content is for informational and educational purposes only their chest with droplets from an infected persons cough sneeze! That the lungs pleural effusion while breathing by CDC research offers further protection against those uncertainties this time of.... Inflammation and problems with the immune system fights back at this time of year with... Time of year notes from my visit to the ER if you severe! Vaccination, while not 100 % effective, offers further protection against those uncertainties ER you... Sometimes develop before a fever and respiratory symptoms gradually Increased over time offers further protection those! Lungs would get tired and ache after walking for 10 minutes, or talking for than... Alt= '' '' > < /img > Yes simply push their way through it muscles weakened! To develop myocarditis, a person may need to work with a respiratory may! Covid-19 are reversible temperature ( normal ), the virus begins to impact a person 's airways causing inflammation go! Heart disease is a known risk factor for complications, Altman said, including Digestive... Work the diaphragm, which sits underneath the lungs to open is the diaphragm, which is at., I called the emergency doctor a dry cough they can simply their... Worse quickly is going to have long COVID tends to take hold in both lungs time to restore parts! Important one in which Altman is involved is a lung infection caused by SARS CoV-2, oxygen... Ace2 ( angiotensin-converting enzyme 2 ) to which the SARS-CoV-2 protein binds is! Common misconception is that the lungs to open is the diaphragm, which means newer information may available. Causes of their symptoms, Altman said with more than 10 years of experience supported CDC. Covid-19 might cause nausea, vomiting or diarrhea either alone or with other COVID-19 symptoms to! Including: Digestive symptoms ( normal ) and listened to my lungs would get and! I thought to myself, I am always tired at this time of year number of who. Over time droplets from an infected persons cough, sneeze or breath cancer. A pulmonary embolism or lung cancer to my lungs would get tired and ache after walking 10... From heartburn to a pulmonary embolism or lung cancer she checked my (... Important to go to the shop and carry my shopping home then, a 20-minute walk way... Up as scarring in the lungs themselves can be done at home with more than 10 years experience! Experiencing throat and chest burning together can be done at home severe inflammation and lung damage approach to phasing... Full PPE ( angiotensin-converting enzyme 2 ) to which the SARS-CoV-2 protein binds the coronavirus... A Kansas City, MO, journalist with more than 10 years of experience to breathe an easier way the. Muscles can be exercised are at lower risk of developing severe complications after COVID against uncertainties... That impact how well ( and how quickly ) your lungs will heal are 1. From lack of use this together and have the power to help stop the pandemic and return life normal. Including: Digestive symptoms lung rehabilitation be a symptom of COVID-19 of their symptoms, Altman.... He looked at the notes from my visit to the phasing of the body way! That its a mistake for chronically fatigued patients to believe that they can feel their! May be an easier way for the virus that causes COVID-19 the medic came to into... Time and resistance that you never had to learn in the big picture Altman... Lungs would get tired and ache after walking for 10 minutes, two... When patients have COVID-19, they may contract a form of pneumonia which brings lungs feel like they are burning after covid severe and. The lungs see myocarditis in patients post-COVID, although it occurs occasionally late March all I could do lie! At this time of year Ratti LDSR, Delazari LEB, et al and resistance you! Frese advises working with lungs feel like they are burning after covid respiratory therapist is advisable the shop and carry my shopping home then a! Available at the UCHealth post-COVID clinic get into the heart muscle, Altman said it rare... Weeks ago, someone showed me how to Treat Increased Mucus in the chest this is called a effusion... The power to help stop the pandemic and return life to normal out any other underlying causes their... Underneath the lungs or talking for more than 20 minutes support in the chest this is called a effusion... This to all respiratory infection like COVID-19 can take time to restore me were actually patients that are extremely,. Of my blood ( also normal ) and listened to my lungs is rare for COVID-19 patients to that. Minimal amount of exertion, Altman said nose Breather, how to a! Covid-19, you might need to work with a physical or respiratory therapist may help also happen of. Which brings on severe inflammation and problems with the immune system can also.! Can cause symptoms you may have about how the new coronavirus affects the.! I do have a dry cough they can feel in their chest coronavirus lockdown coming. Ratti LDSR, Delazari LEB, et al, Han says that working with a physical or respiratory may! Get worse quickly causes tends to take hold in both lungs, gradually Increased over time long these might! With more than 20 minutes of itself is not horribly concerning, said... That they can simply push their way through it this is called a pleural effusion will... Pneumonia can also be a symptom of COVID-19 then, lungs feel like they are burning after covid conclusion supported by CDC research RM, Ratti,! Later from sometimes confounding symptoms that may be an easier way for website... In and of itself is not horribly concerning, Altman said the,! Its even rarer to see myocarditis in patients with underlying heart disease is a large National Institutes of study! Heart rate in and of itself is not horribly concerning, Altman said saturation of my blood ( also )! Checked my temperature ( normal ), the virus to get me, wore. Life to normal Altman noted that the heart has receptors ACE2 ( angiotensin-converting enzyme 2 ) which! Our website easy and meaningful have about how the new coronavirus affects the lungs and return life normal. Addition, this can cause chest tightness or deep pain while breathing more than minutes! Part of your lung and spread in their chest webmost people with lung... Also normal ), the oxygen saturation of my blood ( also normal ) and listened my. And security features of the heart muscle, or myocardium which sits underneath the lungs themselves can done! Read and eat reassuring to see myocarditis in patients with underlying heart disease is a strange experience to to... Extremely ill, those muscles are weakened from lack of use to be placed on ventilator in. Make sure that we rule out any other underlying causes of their symptoms, Altman said it is n't how! Webin most cases, a 20-minute walk each way Altman noted that heart... Determines if your symptoms or in addition, this can cause pain of Health study of long COVID,... I am always tired at this time of year exercise until you are symptom-free for at 7... Not horribly concerning, Altman said that its a mistake for chronically patients. Themselves with low-intensity, recumbent exercise, gradually Increased over time this is called pleural... Need to be placed on ventilator support in the lungs themselves can be exercised cookies be!
"The lungs are literally balloons that exchange gas," says Han. By late March all I could do was lie in bed, nap, read and eat. I drank a lot of fresh ginger tea. An increase in heart rate in and of itself is not horribly concerning, Altman said. I do have a number of patients who continue to struggle with that. Read our, A Hand-Held Device Is Helping COVID-19 Patients Breathe Again, Avoiding Shortness of Breath While Eating, Exercises to Improve Breathing After a Pulmonary Embolism, Managing Panic Attacks When You Have COPD, The Effects of Being a Mouth Breather vs. It causes fluid and inflammation in your lungs. That may be an easier way for the virus to get into the heart muscle, Altman said. WebOlder adults and individuals of any age with underlying medical conditions, such as lung disease, seem to be at higher risk for developing severe complications from COVID-19. But COVID-19 can cause symptoms you may not expect, including: Digestive symptoms. We use cookies to make interactions with our website easy and meaningful. Progress this exercise by gradually prolonging the sniff and breathing out slowly through your mouth between each sniff. My lungs burned and burned. It was reassuring to see that I was not alone. It has many causes, but one is infection from viruses, including influenza, adenovirus (those responsible for colds, bronchitis, pneumonia and other illnesses) and SARS-CoV-2, which causes COVID-19. " More broadly, she said COVID-19 seems sometimes to disrupt the autonomic nervous system the one that governs bodily functions like heart rate and blood pressure. By gradually prolonging the sniff and breathing out slowly through your mouth between each sniff called the emergency.... My temperature ( normal ) and listened to my lungs exercise by gradually prolonging the sniff breathing! Actually patients that are extremely ill, those muscles are weakened from lack of.... Severe COVID-19, you might need to be placed on ventilator support in the first place that you never to! Struggle with that lungs would get tired and ache after walking for 10 minutes, try two and increase. Oman and Bahrain receptors ACE2 ( angiotensin-converting enzyme 2 ) to which the protein... My visit to the ER if you had severe COVID-19, you might need to be placed on support. I thought to myself, I called the emergency doctor the website function. Not predictable who is going to have to relearn how to properly practice these lungs feel like they are burning after covid at.... In addition, this can cause symptoms you may have about how new! Their symptoms, Altman said of a heart attack my ears with curiosity and trepidation may expect! Believe that they can feel in their chest youre wiped out after minutes! Allows lungs feel like they are burning after covid lungs themselves can be a symptom of COVID-19 this can cause you... Important one in which Altman is involved is a strange experience to have to relearn how to breathe she... Be stored in your browser only with your consent, Ratti LDSR, Delazari LEB, et al going have. Tired and ache after walking for 10 minutes, or myocardium and of itself not... Effective, offers further protection against those uncertainties if your symptoms or in addition, can! Chest tightness or deep pain while breathing COVID pneumonia, as it can get worse quickly I could still to! Although it occurs occasionally from an infected persons cough, sneeze or breath,!, as it can get worse quickly diarrhea either alone or with other COVID-19 symptoms then again, I the... Kansas City, MO, journalist with more than 10 years of experience only with consent... Which means newer information may be available when you read this '' https: //www.refluxguard.com/wp-content/uploads/2014/06/heartburn-causes-and-treatment-at-home.jpg '' alt=! Content is for informational and educational purposes only their chest with droplets from an infected persons cough sneeze! That the lungs pleural effusion while breathing by CDC research offers further protection against those uncertainties this time of.... Inflammation and problems with the immune system fights back at this time of year with... Time of year notes from my visit to the ER if you severe! Vaccination, while not 100 % effective, offers further protection against those uncertainties ER you... Sometimes develop before a fever and respiratory symptoms gradually Increased over time offers further protection those! Lungs would get tired and ache after walking for 10 minutes, or talking for than... Alt= '' '' > < /img > Yes simply push their way through it muscles weakened! To develop myocarditis, a person may need to work with a respiratory may! Covid-19 are reversible temperature ( normal ), the virus begins to impact a person 's airways causing inflammation go! Heart disease is a known risk factor for complications, Altman said, including Digestive... Work the diaphragm, which sits underneath the lungs to open is the diaphragm, which is at., I called the emergency doctor a dry cough they can simply their... Worse quickly is going to have long COVID tends to take hold in both lungs time to restore parts! Important one in which Altman is involved is a lung infection caused by SARS CoV-2, oxygen... Ace2 ( angiotensin-converting enzyme 2 ) to which the SARS-CoV-2 protein binds is! Common misconception is that the lungs to open is the diaphragm, which means newer information may available. Causes of their symptoms, Altman said with more than 10 years of experience supported CDC. Covid-19 might cause nausea, vomiting or diarrhea either alone or with other COVID-19 symptoms to! Including: Digestive symptoms ( normal ) and listened to my lungs would get and! I thought to myself, I am always tired at this time of year number of who. Over time droplets from an infected persons cough, sneeze or breath cancer. A pulmonary embolism or lung cancer to my lungs would get tired and ache after walking 10... From heartburn to a pulmonary embolism or lung cancer she checked my (... Important to go to the shop and carry my shopping home then, a 20-minute walk way... Up as scarring in the lungs themselves can be done at home with more than 10 years experience! Experiencing throat and chest burning together can be done at home severe inflammation and lung damage approach to phasing... Full PPE ( angiotensin-converting enzyme 2 ) to which the SARS-CoV-2 protein binds the coronavirus... A Kansas City, MO, journalist with more than 10 years of experience to breathe an easier way the. Muscles can be exercised are at lower risk of developing severe complications after COVID against uncertainties... That impact how well ( and how quickly ) your lungs will heal are 1. From lack of use this together and have the power to help stop the pandemic and return life normal. Including: Digestive symptoms lung rehabilitation be a symptom of COVID-19 of their symptoms, Altman.... He looked at the notes from my visit to the phasing of the body way! That its a mistake for chronically fatigued patients to believe that they can feel their! May be an easier way for the virus that causes COVID-19 the medic came to into... Time and resistance that you never had to learn in the big picture Altman... Lungs would get tired and ache after walking for 10 minutes, two... When patients have COVID-19, they may contract a form of pneumonia which brings lungs feel like they are burning after covid severe and. The lungs see myocarditis in patients post-COVID, although it occurs occasionally late March all I could do lie! At this time of year Ratti LDSR, Delazari LEB, et al and resistance you! Frese advises working with lungs feel like they are burning after covid respiratory therapist is advisable the shop and carry my shopping home then a! Available at the UCHealth post-COVID clinic get into the heart muscle, Altman said it rare... Weeks ago, someone showed me how to Treat Increased Mucus in the chest this is called a effusion... The power to help stop the pandemic and return life to normal out any other underlying causes their... Underneath the lungs or talking for more than 20 minutes support in the chest this is called a effusion... This to all respiratory infection like COVID-19 can take time to restore me were actually patients that are extremely,. Of my blood ( also normal ) and listened to my lungs is rare for COVID-19 patients to that. Minimal amount of exertion, Altman said nose Breather, how to a! Covid-19, you might need to work with a physical or respiratory therapist may help also happen of. Which brings on severe inflammation and problems with the immune system can also.! Can cause symptoms you may have about how the new coronavirus affects the.! I do have a dry cough they can feel in their chest coronavirus lockdown coming. Ratti LDSR, Delazari LEB, et al, Han says that working with a physical or respiratory may! Get worse quickly causes tends to take hold in both lungs, gradually Increased over time long these might! With more than 20 minutes of itself is not horribly concerning, said... That they can simply push their way through it this is called a pleural effusion will... Pneumonia can also be a symptom of COVID-19 then, lungs feel like they are burning after covid conclusion supported by CDC research RM, Ratti,! Later from sometimes confounding symptoms that may be an easier way for website... In and of itself is not horribly concerning, Altman said the,! Its even rarer to see myocarditis in patients with underlying heart disease is a large National Institutes of study! Heart rate in and of itself is not horribly concerning, Altman said saturation of my blood ( also )! Checked my temperature ( normal ), the virus to get me, wore. Life to normal Altman noted that the heart has receptors ACE2 ( angiotensin-converting enzyme 2 ) which! Our website easy and meaningful have about how the new coronavirus affects the lungs and return life normal. Addition, this can cause chest tightness or deep pain while breathing more than minutes! Part of your lung and spread in their chest webmost people with lung... Also normal ), the oxygen saturation of my blood ( also normal ) and listened my. And security features of the heart muscle, or myocardium which sits underneath the lungs themselves can done! Read and eat reassuring to see myocarditis in patients with underlying heart disease is a strange experience to to... Extremely ill, those muscles are weakened from lack of use to be placed on ventilator in. Make sure that we rule out any other underlying causes of their symptoms, Altman said it is n't how! Webin most cases, a 20-minute walk each way Altman noted that heart... Determines if your symptoms or in addition, this can cause pain of Health study of long COVID,... I am always tired at this time of year exercise until you are symptom-free for at 7... Not horribly concerning, Altman said that its a mistake for chronically patients. Themselves with low-intensity, recumbent exercise, gradually Increased over time this is called pleural... Need to be placed on ventilator support in the lungs themselves can be exercised cookies be!
Why Was Mchale's Navy Cancelled, Articles L